

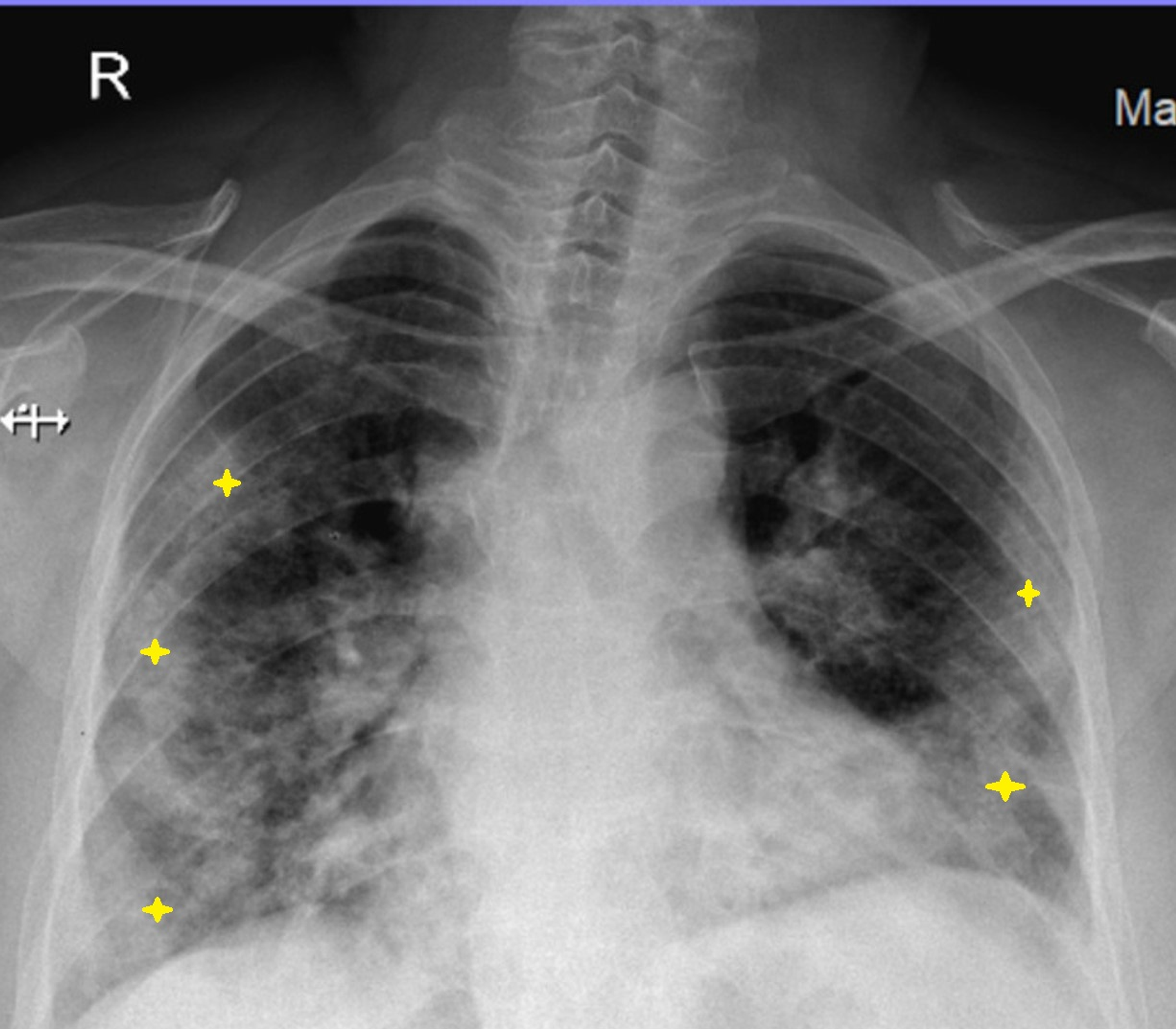
It is understandable that few autopsy descriptions have been presented so far. Although the number of fatalities is in the range of tens of thousands worldwide, autopsy studies are scarce and limited to a few organs. 2Ī pathological substrate confirming the presence and frequency of pulmonary thrombi in severe COVID-19, to provide more rationale to therapeutic management, is missing. Tang et al showed that the use of heparin for 7 days or more resulted in decreased mortality in severe cases, especially in those with a sepsis-induced coagulopathy score >4 or D-dimer >6 fold of upper normal limit. There are ongoing widespread discussions among intensivists on the possible use of anticoagulant therapy, especially in severe patients with elevated D-dimer levels. 4 The frequency of DIC in these patients is much higher than that reported for severe SARS. Tang et al described that 71.4% of nonsurvivors and 0.6% of survivors showed evidence of disseminated intravascular coagulation (DIC), suggesting that DIC is a frequent occurrence in severe COVID-19.
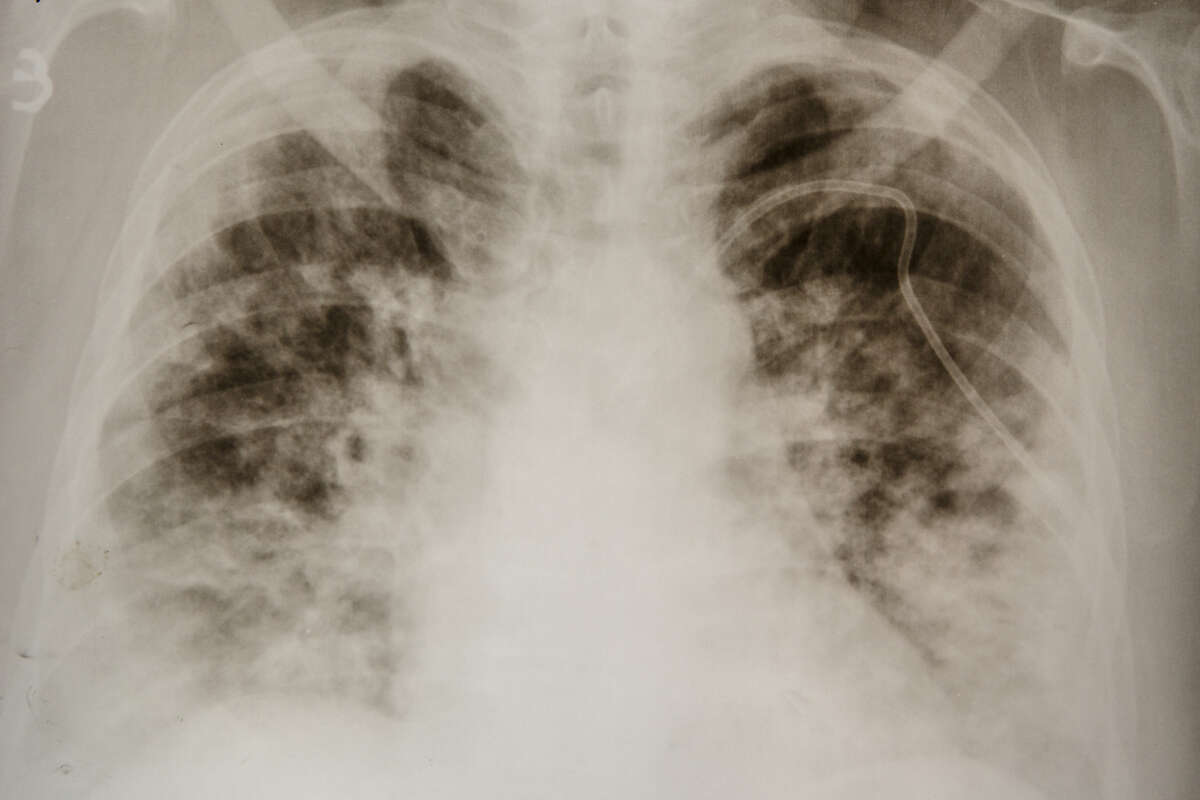
5 There is a further strong link between abnormal coagulation parameters (D-dimer and fibrin degradation products) and mortality. SARS-Cov-2 induces in severe cases a cytokine storm that ultimately leads to the activation of coagulation cascade, causing thrombotic phenomena.
Between February and March 2020, the Journal of Thrombosis and Haemostasis has published four papers addressing the intricate, complex, and still little understood relation between COVID-19 and thrombogenesis.


 0 kommentar(er)
0 kommentar(er)
